Cancer is being diagnosed at earlier ages — and later stages

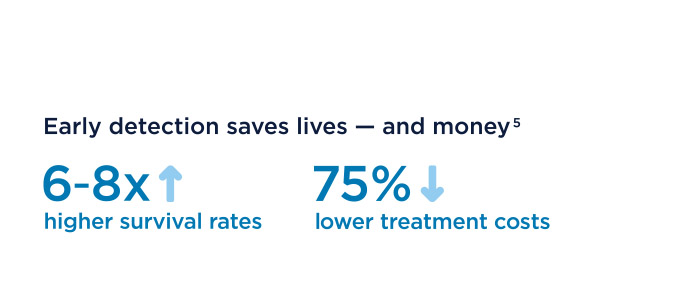
The power of prevention and early cancer detection
Are your employees getting the cancer screenings they need?
Choose the right health plan
Create a work culture that promotes health
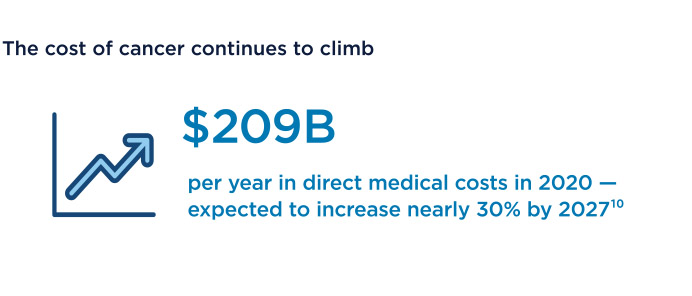
Proactive cancer prevention makes solid business sense
Footnotes:
1“Trends to Watch in 2024,” Business Group on Health, November 28, 2023.
2“U.S. Oncology Survey: Employers Expect Cancer Costs to Spike by Up To 30% in Three Years, Hungry for Value-Based Models,” Carrum Health, February 26, 2024.
3“Cancer Facts and Figures 2024,” American Cancer Society, 2024.
4See note 3.
5“Employer Insights Report 2024,” Color Health, 2024.
6David C. Grabowski et al., “Assessment of Medical and Public Assistance Expenditures and Employment Among US Adults with Cancer Diagnoses,” Journal of the American Medical Association, May 26, 2023.
7See note 1.
8Courtney Vinopal, “Cancer Rates are Rising Among People Under Age 50. Here’s Why Employers Should Care,” HR Brew, October 10, 2023.
9Jianhui Zhao et al., “Global trends in incidence, death, burden and risk factors of early-onset cancer from 1990 to 2019,” BMJ Oncology, 2023.
10See notes 2 and 6.
11Harlan Levine, “Health Care Navigation’s Vital Role in Cancer Care,” ALM Benefits Pro, April 6, 2023.
12See note 11.
13“New Survey Shows Clear Need for Paid Leave Among Cancer Patients and Survivors,” American Cancer Society Cancer Action Network, December 7, 2021.
14Ze Cong et al., “Productivity Loss and Indirect Costs for Patients Newly Diagnosed with Early- versus Late-Stage Cancer in the USA: A Large-Scale Observational Research Study,” Applied Health Economics and Health Policy, August 30, 2022.
15“Risk of Dying from Cancer Continues to Drop at an Accelerated Pace,” American Cancer Society, January 12, 2022.
16See note 5.
17See note 5.
18Michelle Tong et al., “Racial Disparities in Cancer Outcomes, Screening, and Treatment,” Kaiser Family Foundation, February 3, 2022.
19See note 5.
20See note 5.
21See note 5.
22See note 5.
23Zehau Yu, et al., “Assessing the Documentation of Social Determinants of Health for Lung Cancer Patients in Clinical Narratives,” Frontiers in Public Health, March 28, 2022.



 Generate awareness for cancer prevention
Generate awareness for cancer prevention